Understanding Multiple Myeloma: Racial Disparities and Treatment Outcomes
Multiple myeloma (MM) is a complex and formidable plasma cell disorder, notable for its striking racial disparities in both incidence and mortality. The statistics are glaring: in the United States, Black Americans (BA) experience roughly double the rate of incidence and mortality compared to White Americans (WA). This makes MM the most prevalent hematologic malignancy among Black individuals, revealing deep-seated health inequities that require urgent attention.
The Challenge of Access to Care
Access to timely and optimal treatment for MM is a well-documented problem for racial minorities. Numerous studies have highlighted the disparities in treatment accessibility, which contributes to poorer outcomes for Black patients. Yet, the extent to which biological or genetic factors contribute to survival differences among different racial groups remains uncertain. Some research suggests that when treatment access is equitable, Black patients may actually have better or equivalent survival rates compared to their White counterparts.
The Study at the University of Arkansas
At the University of Arkansas for Medical Sciences (UARK), an extensive analysis was conducted involving a diverse patient population. The study included 1,024 BA and 6,941 WA patients diagnosed with myeloma. Only a subset of these, 1,827 patients (171 BA and 1,656 WA), met rigorous inclusion criteria, focusing on newly diagnosed MM, limited prior therapy, and autologous stem cell transplantation (ASCT) within a specific timeframe. By evaluating patient outcomes within this tightly controlled cohort, researchers aimed to glean insights free from the confounding effects of unequal treatment access.
Demographic Insights
Within the UARK-NDMM cohort, notable demographic differences emerged. Black patients were, on average, younger than their White counterparts, with a higher proportion under 50 years old. Interestingly, a larger percentage of the Black cohort were women, reflecting national data that shows Black women have a significantly higher incidence of myeloma than White women.
Baseline clinical differences also emerged, including higher rates of obesity and elevated diastolic blood pressure among Black patients. While some prognostic factors such as disease extent evaluated via advanced imaging and molecular risk profiles were comparable across both groups, the discrepancies in baseline health metrics raise important questions regarding their impact on treatment outcomes.
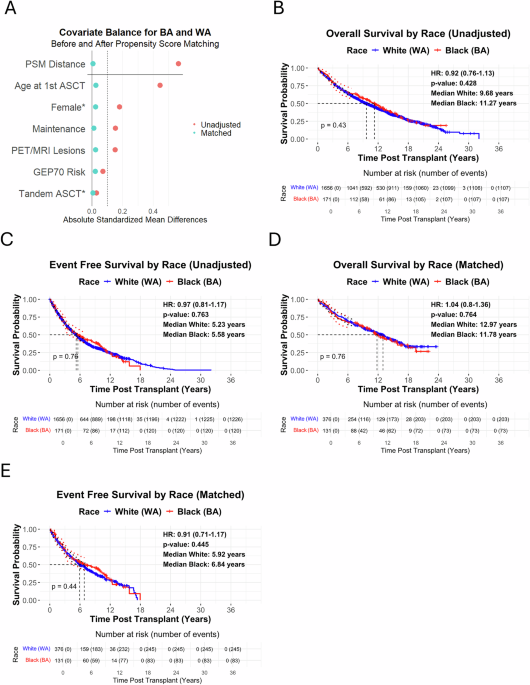
Treatment Matching and Methodology
To minimize the inherent biases presented by demographic disparities, researchers employed Propensity Score Matching (PSM), which paired BA and WA patients based on critical prognostic factors. This methodological rigor aimed to create clinically similar groups, ensuring that comparisons were fair and meaningful. With carefully defined matching criteria, the study could isolate the effects of race from those of other variables impacting treatment and outcomes.
Analyzing Cytogenetic Differences
The study also explored cytogenetic differences, albeit noting that matched differences were modest. For example, the presence of certain chromosomal abnormalities, such as t(11;14), appeared less frequently in Black patients compared to White patients, though other significant abnormalities exhibited similar rates. These findings contribute to the complex narrative of racial differences in MM, underscoring the need for discerning analysis.
Survival Outcomes and Treatments
Analyzing the outcomes, the matched cohort findings revealed comparable survival rates between the two racial groups. In fact, the median overall survival (OS) for Black patients was slightly higher than that of White patients, suggesting that when treated equitably, racial disparities in MM outcomes diminish significantly. This reinforces the hypothesis that systemic improvements in care access could yield substantial benefits for Black patients.
Implications for Future Research
The strengths of this study lie not only in its comprehensive data evaluations but also in its commitment to rigorously controlled comparisons. By scrutinizing treatment matching alongside demographic factors, it emphasizes a broader narrative: addressing racial disparities in healthcare necessitates thoughtful, data-informed approaches that consider both biological and social determinants of health.
Paths Forward in Cancer Care
As the healthcare community grapples with these complexities, the findings advocate for systemic strategies that weave together clinical and socioeconomic factors. Enhanced risk stratification through advanced diagnostics, including molecular profiling and state-of-the-art imaging, could prove instrumental in leveling the playing field for all patients battling multiple myeloma.
This ongoing research serves as a clarion call to ensure that every patient, irrespective of their racial background, receives the optimal care and support they deserve. Future investigations should adopt similar rigorous methodologies, shedding light on how best to integrate equity into cancer care and improve outcomes across diverse populations.