Stark Racial Disparities in Maternal and Infant Health in the U.S.
Summary
Despite advancements in medical care, racial disparities in maternal and infant health outcomes in the United States remain a pressing public health crisis. The U.S. has the highest rate of maternal deaths among high-income nations, with stark contrasts evident when looking at the statistics for different racial and ethnic groups. The COVID-19 pandemic particularly highlighted these disparities, drawing attention to inequities in maternal and infant health care.
Key changes in policies, such as the overturning of Roe v. Wade, growing barriers to abortion access, and cuts to health program funding may further inflate the existing inequalities in maternal health care. This brief explores the data surrounding these disparities, the underlying factors contributing to them, and recent policy actions that have the potential to widen the gap.
Racial Disparities in Maternal and Infant Health
Pregnancy-Related Mortality Rates
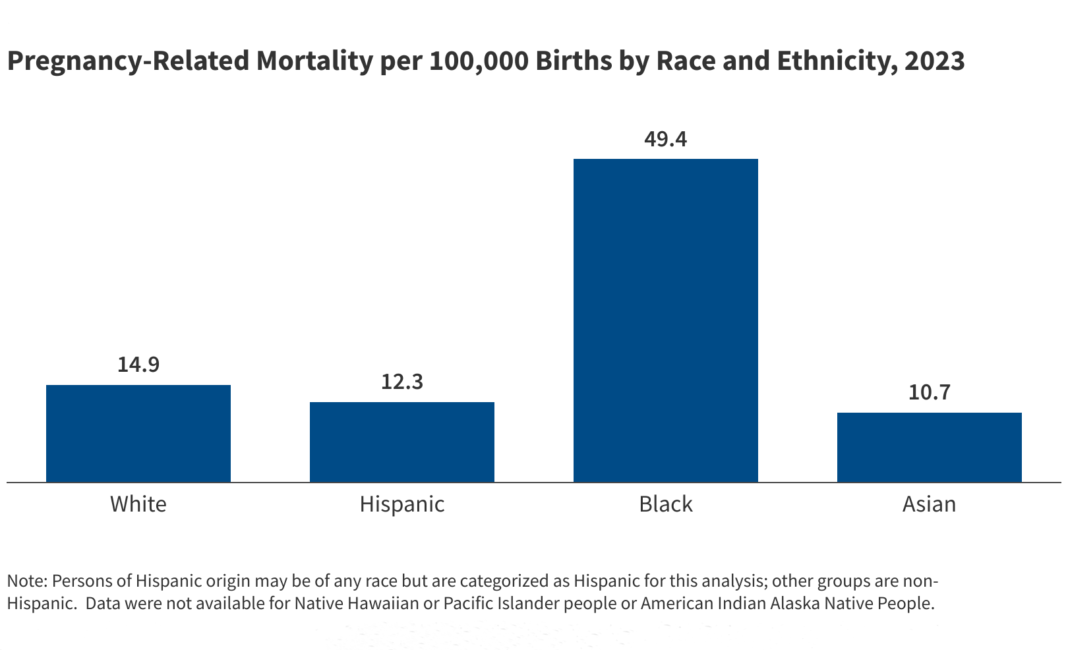
In 2023, approximately 676 women in the U.S. lost their lives due to complications related to pregnancy, marking a decrease from 793 maternal deaths in 2022. However, while pregnancy-related mortality rates showed improvement among White and Hispanic women, Black women continue to be disproportionately affected. The pregnancy-related mortality rate for Black women is over three times that of White women, with 49.4 deaths per 100,000 live births compared to 14.9 for their White counterparts. Alarmingly, earlier data illustrates that American Indian or Alaska Native (AIAN) and Native Hawaiian/Pacific Islander (NHPI) individuals may have even higher mortality rates.
Factors such as age, education, and social determinants contribute to this disparity. Black women with college degrees are still more likely to experience mortality than White women with lower education levels. The risk of severe maternal morbidity is significantly heightened in these populations, emphasizing how systemic issues intertwine with health outcomes.
Birth Risks and Outcomes
Disparities in birth risks highlight the challenges faced by many Black, AIAN, and NHPI women compared to White women. Factors like preterm birth and low birthweight, which significantly contribute to infant mortality, are more prevalent in these groups. Remarkably, NHPI women are four times more likely to receive late or no prenatal care during their pregnancies.
Teen birth rates offer another layer of disparity; while they have declined overall, they remain higher among non-White teens. Unplanned pregnancies often lead to inadequate prenatal care, creating a ripple effect that can influence both the immediate and long-term health of both mothers and infants.
Infants born to AIAN, Black, Hispanic, and NHPI mothers show higher mortality rates compared to those born to White mothers, further linking these disparities directly to maternal health outcomes.
Factors Driving Disparities in Maternal and Infant Health
The complexities behind these disparities encompass a wide range of social and economic factors that extend beyond mere access to healthcare. Linguistic and cultural barriers, entrenched racism, and lack of availability of quality care in their communities compound the challenges faced by these populations.
Recent research has begun to focus on the concept of reproductive justice, highlighting how various social determinants—like income, education, and community safety—intersect and influence health outcomes. While Hispanic women may fare better than others despite facing barriers, the so-called Hispanic paradox is still not fully understood, indicating the need for further exploration.
In regions such as the South, where large populations of Black individuals reside, access to obstetric care is alarmingly limited. The rise in hospital and obstetric unit closures heightens the risk for Black infant health, revealing an urgent need for more accessible care solutions.
Current Policies Impacting Maternal and Infant Health Disparities
Recent governmental policy changes have introduced new challenges to maternal health care. The rollback of federal diversity initiatives under the Trump administration has created fears of a potential widening of existing disparities. Efforts to strengthen maternal health equity are hampered by funding cuts and reductions in key healthcare programs.
The 2025 tax and spending legislation includes substantial reductions in federal Medicaid spending, a vital source of healthcare coverage for many communities of color. This has left individuals at risk of losing their healthcare access during critical times in their lives.
Additional restrictions on family planning services, particularly concerning organizations like Planned Parenthood, threaten essential health resources that serve low-income women and communities of color. Therefore, as funding cuts to essential healthcare services deepen, the resources available to support maternal and infant health will likely dwindle.
Abortion restrictions that arose following the Dobbs ruling further complicate access to necessary healthcare, disproportionately affecting marginalized communities already at higher risk for pregnancy-related complications.
Without significant policy interventions and a commitment to addressing these disparities, improvements in maternal and infant health equity will remain elusive, leaving community members vulnerable and unnecessarily at risk.